|
Research Article
Minimally invasive approach in aortic valve replacement: Techniques, patient’s selection, and early post-operative outcomes
1 Cardiovascular Surgery Department, Mohammed VI University Hospital, Marrakech, Morocco
Address correspondence to:
Issaka Zallé
CHU Mohammed VI, BP 2360, Avenue Ibn Sina, Marrakech, MA 40080,
Morocco
Message to Corresponding Author
Article ID: 100020C04IZ2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Zallé I, Son M, Nijimbere M, Boumzebra D. Minimally invasive approach in aortic valve replacement: Techniques, patient’s selection, and early postoperative outcomes. Edorium J Cardiothorac Vasc Surg 2021;8:100020C04IZ2021.ABSTRACT
Aims: In our department, heart valves surgery is routinely performed with conventional full sternotomy. This study aims to report our experience in minimally invasive technique with reference to patient selection, surgical techniques, and early post-operative outcomes.
Methods: Eighteen (18) patients undergoing aortic valve surgery for isolated aortic valve disease were analyzed prospectively from November 2017 to October 2019 in our institution. All patients underwent isolated aortic valve replacement.
Results: The mean age of the patients was 48.4 [28–69] years and 76.4% were male; mean weight was 63.8 [56–82] kg. The average New York Heart Association (NYHA) was 2.4 [1–3]. There were 3 cases of mellitus diabetes, 2 cases of arterial hypertension. Heart function was good in all patients (left ventricular ejection fraction, LVEF 58.3% [35–73]). Pre-operative hemoglobin was 13.9 [10.9–15.3] g/dL [15.7] g/dL. Right anterior mini-thoracotomy with femoro-femoral cannulation for cardiopulmonary bypass (CPB) and upper mini-sternotomy (UMS) were our surgical approaches. There was no conversion to full sternotomy. The mean CPB time and aortic cross-clamp (ACC) time were respectively 131 and 81 minutes, 16.7% of patients required intra and post-operative red blood cells transfusion, post-operative hemoglobin was 11.78 [7.3–14.4] g/dL and 16.7% had needed inotropic support. Mean ventilation time was 2.35 [1–12] hours, and mean time of intensive care unit (ICU) stay was 2.44 [1–8] days; length of hospital stay at 6.5 [5–10] days. The length of chest drains stay was 1.53 [1–2] days. One (1) patient developed cerebrovascular event; there was no in-hospital and 30-days mortality and no wound infections.
Conclusion: Minimally invasive aortic valve replacement (MIAVR) can be adopted as a new surgical approach for aortic valve replacement. Both the surgical access don’t compromise operative outcomes. Otherwise comparative study with conventional full sternotomy is necessary in order to establish the interest of MIAVR.
Keywords: Aortic valve replacement, Early outcomes, Minimally invasive
INTRODUCTION
The prevalence of aortic valve disease is 2% of the general adult population and surgical aortic valve replacement is the main treatment for symptomatic patients [1]. Nowadays surgical treatment includes conventional sternotomy and minimally invasive techniques. The first one is the traditional approach and provides an excellent long-term outcome for patients with surgical indication. To date, this approach remains the gold standard especially for patients at a low or intermediate risk for perioperative mortality [2]. The second is the minimally invasive aortic valve replacement (MIAVR) which was first described by Cosgrove and Sabik in 1996 [3]. Its interest is based on its probable equivalent or superior outcomes compared with conventional aortic valve replacement (CAVR).
This study aimed to report our experience in MIAVR through a right anterior mini-thoracotomy (RAMT) and an upper mini-sternotomy (UMS). We describe our surgical technique, patient’s selection, and early post-operative outcomes.
MATERIALS AND METHODS
This study was a prospectively collected data from 18 patients with aortic valve disease who underwent isolated aortic valve replacement from November 2017 to October 2019 at the Department of Cardiovascular Surgery, Mohammed VI University Hospital.
Optimum patient selection is essential for MIAVR and some main criteria must be considered in order to perform safely surgical procedure. Our pre-operative planning included clinical assessment, chest X-ray, transthoracic echocardiography (TTE), and electrocardiogram (ECG) assessment. Coronary angiography was done in the patients with heart risks factors. Peripheral femoral Doppler was performed in intra-operative. Our exclusion criteria were emergency cases; patients with aortic root dilation, patients with an unfavorable anatomy, and serious lung disease. Patients requiring concomitant procedures such as coronary artery bypass grafting, or other valves surgery, aortic surgery were excluded. Patients undergoing aortic valve repair were also excluded. Patients with moderate obesity were not excluded in our study.
Peri-operative and 30 days follow-up data were collected prospectively and analyzed.
SURGICAL TECHNIQUES
Our techniques are not different from those described in the literature. About right mini-thoracotomy (RMT) a 4–6 cm skin incision was placed at the level of the 3rd intercostal space. Soft tissues dissection was performed and the right mammary artery and vein were ligated and sectioned. Five-millimeter endoscopic trocars were introduced through the 4th and 6th intercostal space at the level of the anterior axillary line and another one in the 5th intercostal space at the level of the middle axillary line in order to perform aortic cross clamping and camera utilization. A soft tissue retractor was used to exposure operative field, cartilage or rib was intact. Femoral-femoral CPB was used either with percutaneous techniques or small groin incision. The majority of cases used mild hypothermia to normothermia CPB. Pericardiotomy was performed 3–4 cm anterior and parallel to the phrenic nerve, extending inferiorly toward the diaphragm and superiorly to the pericardial reflection. The operative field is insufflated with carbon dioxide gas. The ascending aorta is clamped with a low-profile aortic cross-clamp and antegrade cold blood cardioplegia is delivered directly into the ascending aorta by a needle vent catheter. The aortic valve is replaced as usual; adapted instruments are utilized. After weaning CPB, the femoral cannula is removed. A small chest drainage tube is inserted in the right pleural space. The pericardium is approximated and the chest incision is closed.
The other surgical access was an UMS. It is achieved through 6–10 cm midline vertical skin incision, performing a partial J sternotomy at the 3rd to 5th intercostal space. The pericardium is opened vertically and suspended laterally through the skin. Standard cannulation of the ascending aorta was performed directly through the incision. Venous cannulation was performed either via the right atrial appendage in the vast majority of our patients or with femoro-femoral cannulation via a 2 cm groin incision. Myocardial protection and aortic valve replacement were performed as usual fashion. Left ventricle venting was placed through the aortic root or via the right superior pulmonary vein. After CPB initiation, aortic cross-clamp was performed in standard manner. A transverse aortotomy was placed higher. Temporary epicardial wires were fixed and chest tubes drainage was inserted below the low limit of the incision.
RESULTS
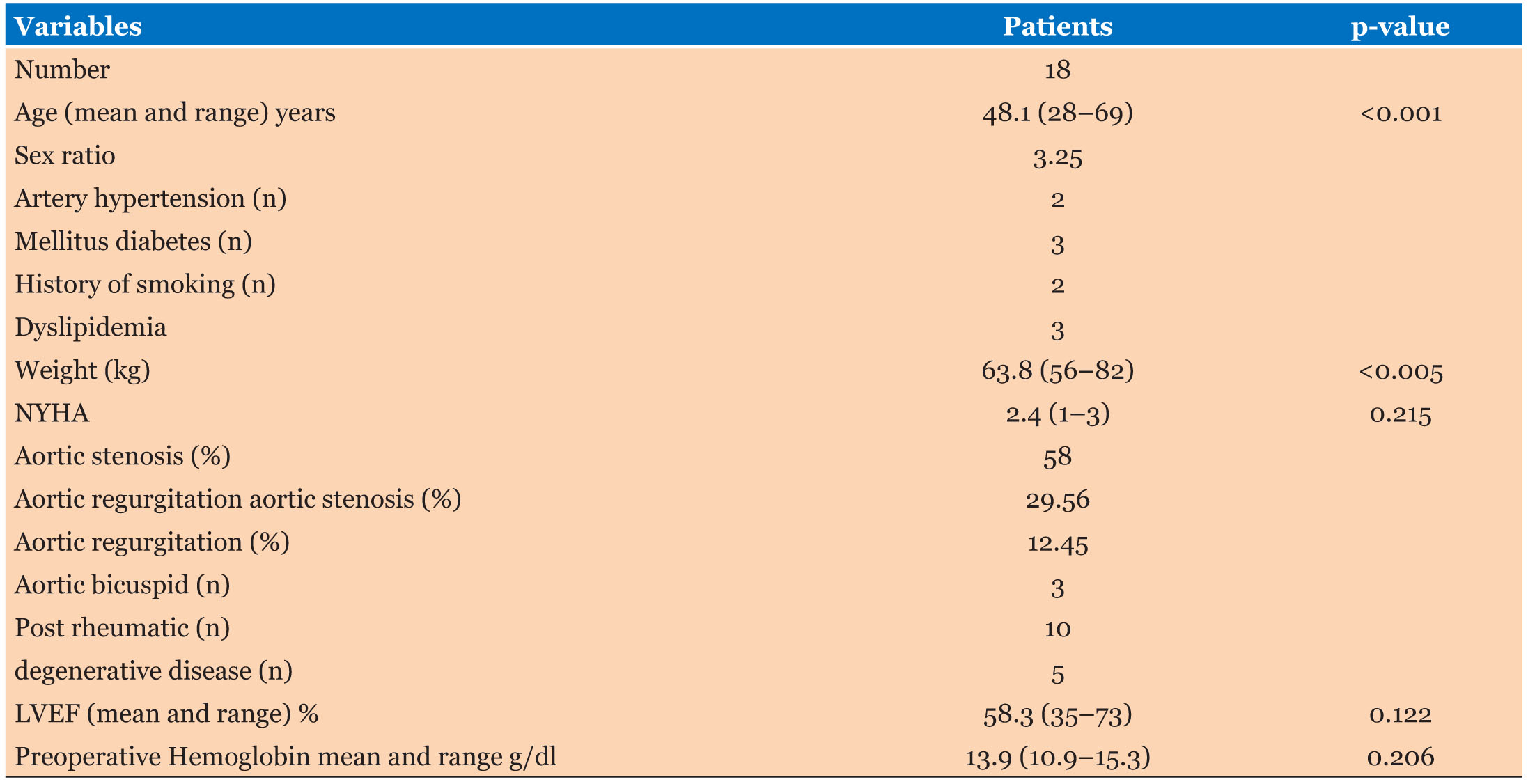
Pre-operative data (Table 1)
The mean age of the patients was 48.4 years and 76.4% were male. The mean weight was 63.8 kg. The average New York Heart Association was 2.4. In term of heart risks factors, 3 cases of mellitus diabetes, 2 cases of artery hypertension, and 2 patients with history of smoking were recorded. The majority of the patients had good heart function, and the mean LVEF was 58.3%. Valve lesions were dominated by valve stenosis (14 patients). The average of mean aortic valve pressure gradient was 43.5 mmHg. The dominant causes were post-rheumatic valve disease (10 patients), 3 patients were diagnosed with bicuspid aortic valve disease, and 5 degenerative disease. Blood analysis showed 13.9 g/dL as mean hemoglobin.
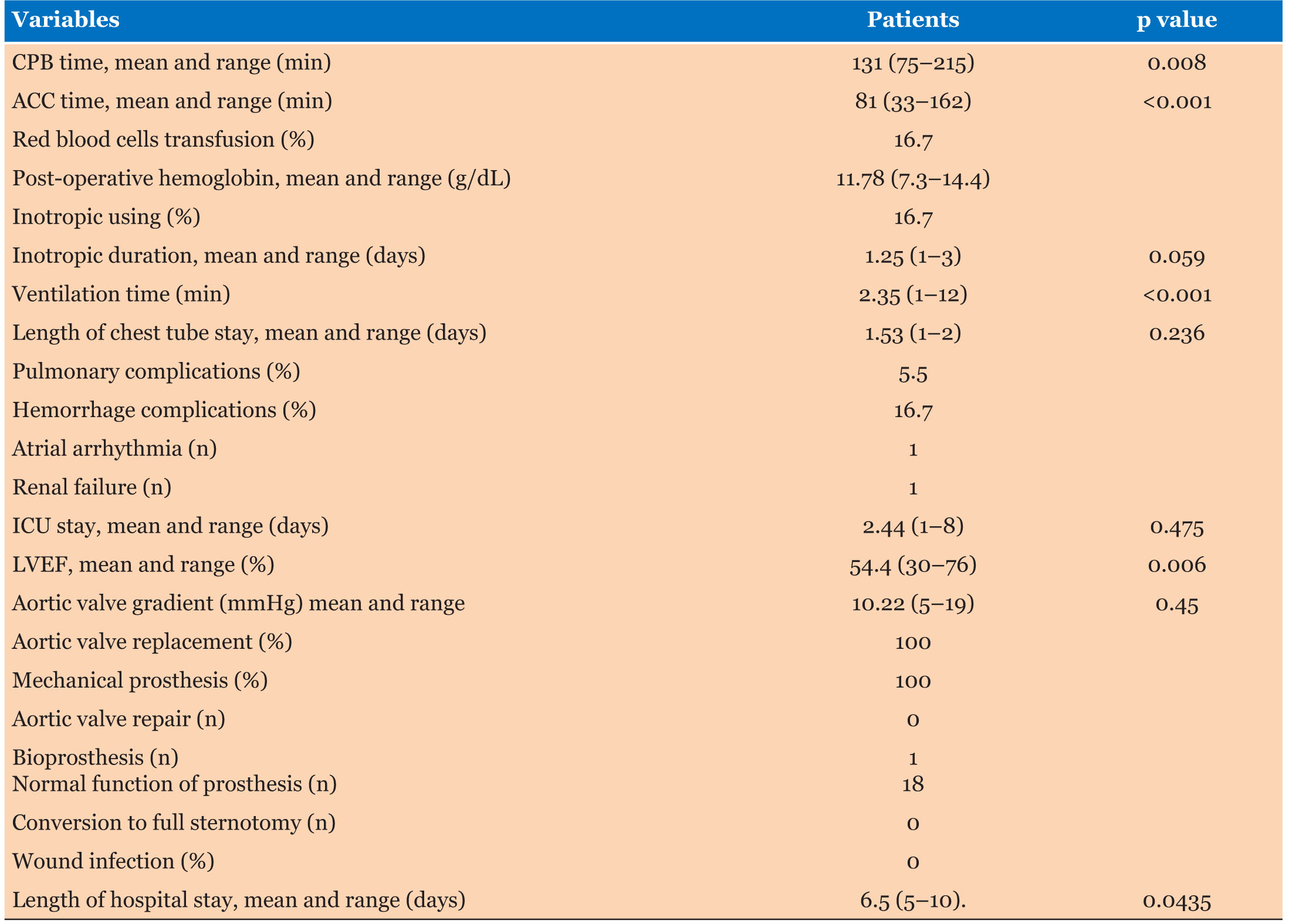
Intra and Post-operative data (Table 2)
Of 18 patients, UMS approach was used in 12 patients and RMT in 6 patients. The surgical procedure was successful in all patients. Seventeen (17) patients received a bileaflet mechanical prosthesis and one (1) bioprosthetic valve (bovine pericardial). The mean CPB and ACC time were respectively 131 and 81 minutes. In our series 16.7% of patients required intra- and post-operative red blood cells transfusion and 16.7% had needed inotropic support administration for mean duration of 1.25 days. The mean ventilation time was 2.5 hours, and the mean time of ICU stay at 2.4 days, length of hospital stay was 6.5 [5–10] days. The length of chest tube stay was 1.53 [1–2] days.
Pre-discharge transthoracic echocardiography (TTE) showed 10.2 mmHg as an average mean aortic valve pressure gradient, mean LVEF at 54.4%. Post-operative mean hemoglobin before transfusion was 11.78 g/dL, one (1) patient had a functional renal failure but returned normal after intensive care. Otherwise no sternal wound infections and no atrio-ventricular bloc were recorded.
DISCUSSION
Most of the patients in our series were younger 48.4 [28–69] years, mean weight was 63.8 kg; LVEF was 58.3% [35–73]. High comorbidity factors were not recorded. Bakir et al. [4], Glower et al. [5], Glauber et al. [6] reported elderly patients, respectively 70, 65, and 69.5 years as a mean age.
According to the literature, the ideal patient for MIAVR may depend to the surgeon opinion. In fact, some surgeons use the minimally invasive surgery approach in all patients. However others use full sternotomy approach in virtually all patients. Other surgeons prefer to use patients with a normal body mass index or a high risk of deep sternal wound infection rather in younger patients [7].
According to certain authors, the main factors to be considerate in this approach include individual surgeon preference and skill sets, the patient’s anatomical factors and comorbidities [8]. High-risk patients may not be good candidates for minimally invasive surgery (MIVS) because the likely longer duration of the surgical procedure of MIVS [9]. Until to date, there is no clear data guiding clinical practice about patient’s selection in MIAVR [10]. Our experience suggests that MIAVR can be used in young patients without high operative risk.
Over the last decade, different minimally invasive surgical approaches for aortic valve replacement exist including upper or lower mini-sternotomy, right parasternal mini-thoracotomy, and transverse sternotomy [11].
We performed in our institution, an UMS and a RAMT. In our series the UMS was more used than RAMT (12 vs. 6 cases). In the study of Nguyen et al. [12], UMS was used in all the patients. Bakir et al. [4] have also used an UMS. Many reports have showed advantages of all these different types of minimally invasive access [11].
Recent studies have demonstrated that mini-sternotomy approach for aortic valve operation is associated with many advantages: a shorter ventilation time, ICU time, hospital stay, and less blood loss [3].
Glauber et al. [9] in their 192 patient series reported 0.7% in-hospital mortality and showed that, compared to mini-sternotomy, right anterior mini-thoracotomy patients had lower post-operative atrial fibrillation (19.5% vs. 34.2%), shorter ventilation time (median 7 vs. 8 h), and a shorter hospital stay (median 5 vs. 6 days). Upper mini-sternotomy and RAMT approaches should be a gold standard in minimally invasive aortic valve surgery (MIAVS).
In our study we did not notify any wound infections, the incidence of red blood cells transfusion was 16.7% with mean post-operative hemoglobin at 11.78 g/dL versus 13.9 in pre-operative. The time ICU stay was 2.4 [1–8] days, ventilation time at 2.35 [1–12] hours. The length of hospital stay was 6.5 [5–10] days. Our observations are consistent with certain series. In fact, Glauber et al. [6] reported incidence of red blood cells transfusion at 18.8%, cerebrovascular events at 1.6%, hospital stay 5 [4–6] days, ICU stay 6 [5–9] hours, with any wound infections. Young et al. [13] who reported in meta-analysis 36% as an incidence of red blood cell transfusion and in the same study the ICU stay and ventilation time were respectively 0.6 [0.25–0.95] days and 4.05 [2.23–5.87] hours. This study reported 1.9% of mortality, and cerebrovascular events in 1%, without deep wound infection. Plass et al. [14] reported cerebrovascular in 3.8%, length of hospital stay 10±3 days, ICU stay 2±2 days, no wound infection. Glower et al. [5] reported cerebrovascular in 1.6%, hospital stay 5 [4–6] days no wound infections. In our study, 5.5% (1 patient) had minor cerebrovascular events, 5.5%. The studies cited above have mentioned cerebrovascular events. That means the MIAVR should be associated with cerebrovascular events. The reduced surgical field with its theoretically inadequate de-airing was advocated as the main cause for possible negative neurologic outcomes. Although early series seem to suggest an increased cerebrovascular events rate, the use of transesophageal echocardiography and continuous CO2 insufflation has recently allowed the achievement of comparable outcomes [15].
In our series post-operative LVEF was conserved and the median was 54.4% [30–76]. Moreover, post-operative aortic valve pressure mean gradient was normal whose 10.22 [5–19] mmHg as a median. Plass et al. [14], Glower et al. [5], Brinkman et al. [16], Glauber et al. [6] reported respectively 63.4%, 55.6%, 55.6%, and 57.9%. Minimally invasive aortic valve surgery is safe and does not compromise post-operative left ventricular function.
The mean aortic cross-clamp time in our study was 81 [33–162] minutes; the mean CPB time was 131 [75–215] minutes. Our observations corroborate with the literature: Mihaljevic et al. [15] reported time 110 [45–368] minutes as a median CPB and median aortic cross-clamp time at 77 [21–291] minutes. Nguyen et al. [12] reported 106.8 minutes as mean aortic cross-clamp time and 153.6 minutes as mean CPB time.
CONCLUSION
Minimally aortic valve replacement through right anterior mini-thoracotomy or upper mini-sternotomy can be adopted as a new surgical approach. Both the surgical access don’t compromise operative outcomes. Young patients without high operative risk can be candidates for MIAVR. Otherwise comparative study with full sternotomy is necessary and may allow to establish the interest of minimally invasive aortic valve replacement.
REFERENCE
1.
Castrovinci S, Emmanuel S, Moscarelli M, et al. Minimally invasive aortic valve surgery. J Geriatr Cardiol 2016;13(6):499–503. [CrossRef]
[Pubmed]

2.
Brown ML, McKellar SH, Sundt TM, Schaff HV. Ministernotomy versus conventional sternotomy for aortic valve replacement: A systematic review and meta-analysis. J Thorac Cardiovasc Surg 2009;137(3):670–9. [CrossRef]
[Pubmed]

3.
Cosgrove DM 3rd, Sabik JF. Minimally invasive approach foraortic valve operations. Ann Thorac Surg 1996;62(2):596–7.
[Pubmed]

4.
Bakir I, Casselman FP, Wellens F, et al. Minimally invasive versus standard approach aortic valve replacement: A study in 506 patients. Ann Thorac Surg 2006;81(5):1599–604. [CrossRef]
[Pubmed]

5.
Glower DD, Lee T, Desai B. Aortic valve replacement through right minithoracotomy in 306 consecutive patients. Innovations (Phila) 2010;5(5):326–30. [CrossRef]
[Pubmed]

6.
Glauber M, Miceli A, Gilmanov D, et al. Right anterior minithoracotomy versus conventional aortic valve replacement: A propensity score matched study. J Thorac Cardiovas Surg 2013;145(5):1222–6. [CrossRef]
[Pubmed]

7.
Peters WS, Smith JA, Preovolos A, Rabinov M, Buckland MR, Rosenfeldt FL. Mitral valve replacement via a right mini-thoracotomy in the dog: Use of carbon dioxide to reduce intracardiac air. Eur J Cardiothorac Surg 1997;11(6):1067–73. [CrossRef]
[Pubmed]

8.
Khan I, Smith JA, Trehan N. Minimally invasive right anterior mini-thoracotomy aortic valve replacement. 2019. [CrossRef]

9.
Glauber M, Miceli A, Bevilacqua S, Farneti PA. Minimally invasive aortic valve replacement via right anterior minithoracotomy: Early outcomes and midterm follow-up. J Thorac Cardiovasc Surg 2011;142(6):1577–9. [CrossRef]
[Pubmed]

10.
Attia RQ, Hickey GL, Grant SW, et al. Minimally invasive versus conventional aortic valve replacement: A propensity-matched study from the UK National Data. Innovations (Phila) 2016;11(1):15–23. [CrossRef]
[Pubmed]

11.
von Segesser LK, Westaby S, Pomar J, Loisance D, Groscurth P, Turina M. Less invasive aortic valve surgery: Rationale and technique. Eur J Cardiothorac Surg 1999;15(6):781–5. [CrossRef]
[Pubmed]

12.
Nguyen DH, Vo AT, Le KM, et al. Minimally invasive Ozaki procedure in aortic valve disease: The preliminary results. Innovations (Phila) 2018;13(5):332–7. [CrossRef]
[Pubmed]

13.
Young CP, Sinhab S, Vohrab HA. Outcomes of minimally invasive aortic valve replacement surgery. Eur J Cardiothorac Surg 2018;53(suppl_2):ii19–23. [CrossRef]
[Pubmed]

14.
Plass A, Scheffel H, Alkadhi H, et al. Aortic valve replacement through a minimally invasive approach: Preoperative planning, surgical technique, and outcome. Ann Thorac Surg 2009;88(6):1851–6. [CrossRef]
[Pubmed]

15.
Mihaljevic T, Cohn LH, Unic D, Aranki SF, Couper GS, Byrne JG. One thousand minimally invasive valve operations: Early and late results. Ann Surg 2004;240(3):529–34. [CrossRef]
[Pubmed]

16.
Brinkman WT, Hoffman W, Dewey TM, et al. Aortic valve replacement surgery: Comparison of outcomes in matched sternotomy and PORT ACCESS groups. Ann Thorac Surg 2010;90(1):131–5. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Issaka Zallé - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Moussa Son - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Macedoine Nijimbere - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Drissi Boumzebra - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Issaka Zallé et al. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.