|
Research Article
Right anterior mini-thoracotomy in mitral valve surgery: Techniques, patients selection, and early post-operative outcomes
1 Cardiovascular Surgery Department, Mohammed VI University Hospital, Marrakech, Morocco
Address correspondence to:
Issaka Zallé
Cardiovascular Surgery Department, Mohammed VI University Hospital, Marrakech,
Morocco
Message to Corresponding Author
Article ID: 100021C04IZ2021
Access full text article on other devices

Access PDF of article on other devices

How to cite this article
Zallé I, Son M, Nijimbere M, El Mardouli M, Boumzebra D. Right anterior mini-thoracotomy in mitral valve surgery: Techniques, patients selection, and early postoperative outcomes. Edorium J Cardiothorac Vasc Surg 2021;8:100021C04IZ2021.ABSTRACT
Aims: In our department, heart valves surgery is performed usually through a full sternotomy. Few years ago we did some experience in minimally invasive valve surgery. That is why we aim to report our experience in minimally invasive mitral valve surgery with reference to patients selection, surgical techniques, and early post-operative outcomes.
Methods: A total of 26 patients undergoing mitral valve surgery for isolated mitral valve disease were analyzed prospectively from November 2017 to October 2019 in our department. All the patients underwent isolated mitral valve surgery.
Results: Our patients were younger, 48.6 [26–66] years, mean weight 56.8 [46–76] kg, sex-ratio at 0.44. The average New York Heart Association was 2.39 [1–3]. They had not heart risks factors. The left ventricular function was good, mean left ventricular ejection fraction (LVEF) was 60.5% [44.5–72], and the mean pulmonary hypertension was 37 [17–89] mmHg. The electrocardiogram showed 38.5% of atrial arrhythmia; the mean pre-operative haemoglobin was 13.6 [11.9–15.7] g/dL. Right anterior mini-thoracotomy with femoro-femoral cardiopulmonary bypass (CPB) was the surgical technique in all the patients. Valve replacement was performed in 84.6% of cases. Three (3) patients underwent mitral valve repair. There were no conversion to full sternotomy and no major complications. The incidence of red blood cells transfusion was 12.2%, mean post-operative hemoglobin at 10.6 [8.1–13.6] g/ dL before transfusion. Heart dysfunction was not found in this study (19% needed inotropic support using and average duration was 1.5 [1–3] hours). The mean CPB time was 161 minutes, aortic cross clamp (ACC) time was 99 minutes. In addition, the mean ventilation time was 3.05 [1–6] hours, length of chest drain stay at 1.38 [1–2] days, mean time of ICU stay at 1.1 [1–6] days, the length of hospital stay 6.9 [6–16] days. Post-operative LVEF was 55.25% [48–68]. There were no chest wound infection, no atrial or ventricular arrhythmia. However, 11.5% of the patients had minor cerebrovascular events and 11.5% had pleural effusion. Moreover, we notified one in-hospital death due to pulmonary failure.
Conclusion: Minimally mitral valve surgery by right anterior mini-thoracotomy can be performed safely without additional operative complications. It may improve early post-operative outcomes. A comparative study with conventional full sternotomy is necessary in order to establish the interest of this new approach.
Keywords: Early outcomes, Full sternotomy, Mitral valve repair, Mitral valve surgery, Right anterior minithoracotomy
INTRODUCTION
Nowadays in mitral valve surgery, different choice of surgical options exists for surgeons and patients. Notably, advances in imaging and surgical instrumentation allow surgeons to perform less invasive incisions.
Minimal invasive approaches have been used with increasing frequency for heart valve repair and replacement over the past 10 years [1],[2]. According to the literature [3], it may lead to inferior results particularly for mitral valve surgery (MVS) due to the small operative field, the need for specialized equipment and operative tools, and the need for special surgeon training. Despite this concern, minimally invasive mitral valve surgery (MIMVS) continued to progress with various technological innovations. As a result, MIMVS is increasingly used, and allows minimally invasive mitral valve repair in the asymptomatic population [4].
In addition, an adequate pre-operative assessment and planning of the approach allow performing surgical procedure uneventful.
This study aimed to report our experience MIMVS through a right anterior mini-thoracotomy (RAMT) approach and describes surgical technique, patient selection, and early post-operative outcomes.
MATERIALS AND METHODS
A total of 26 patients underwent mitral valve surgery for mitral valve disease were analyzed prospectively from November 2017 to October 2019 at the Department of Cardiovascular Surgery, Mohammed VI Medical University.
Patient’s selection is essential to perform uneventful MIMVS. Our pre-operative management was based on clinical and radiology assessment. The exclusion criteria were emergency cases, patients with aortic root diseases, patients included an unfavorable anatomy, and serious lung disease. Patients requiring concomitant procedures such as coronary artery bypass grafting, other valves surgery were excluded. Pre-operative investigations included chest X-ray, transthoracic echocardiography (TTE), and electrocardiogram (ECG). Coronary angiography in patients with heart risks factors was performed. We did not perform computed tomography scan but peripheral femoral vessels exploration with ultrasound Doppler were performed in intra-operative. Pre-discharge TTE and chest radiography were also recorded in all the patients. Peri-operative characteristics including operative variables, postoperative outcomes (early events within 6–16 days), and 30-day follow-up were collected prospectively.
Surgical techniques
Much surgical access such as upper hemi-sternotomy technique, lower hemi-sternotomy technique, right parasternal approach, right mini-thoracotomy approach has been described to perform MIMVS. Right anterior mini-thoracotomy became the primary approach in current MIMVS, increasing the popularity of MIMVS [5]. All these minimally invasive techniques are associated with improvement post-operative outcomes including less invasive surgical techniques, faster recovery time, and improved cosmetic results.
Of these different approaches our department had adopted right mini-thoracotomy technique. Our techniques were not different to those described in the literature.
The patients were induced under general anesthesia in the supine position and monitoring lines were placed. Endotracheal double lumentube was use for intubation and during the intervention selective ventilation was performed through the double lumen tube. Cardiopulmonary bypass was instituted via femoral arterial and venous cannulation through 3–4 cm transverse incisions in the right groin. The venous cannula was positioned under trans-oesophageal echocardiographic (TOE) guidance in the right atrium. The majority of cases used mild hypothermia to normothermia CPB. A right lateral mini-thoracotomy, 5–6 cm incision was made in the anterior axillary line of the 4th intercostal space just superior to the submammary crease. The right lung is deflated to access the pleural cavity, and then soft tissue retractor is placed in the wound. Cardiopulmonary bypass was used throughout the procedure. A video camera was inserted through a 10 mm port in the right 2nd intercostal space and a transthoracic Chitwood aortic cross-clamp was inserted through a 5 mm incision in the 3rd intercostal space [6]. Antegrade cold blood cardioplegia was administered directly into the aortic root. The surgical field was flooded with carbon dioxide through the camera port. The left atrium was opened posterior to the interatrial groove. A left atrial retractor was used to expose the mitral valve. Specialized surgical tools were used. Usually mitral valve surgery techniques were employed. Mitral valve repair procedures were performed following Carpentier techniques [5],[6],[7]. A temporary right ventricular pacing wire was placed before removing aortic cross clamp.
RESULTS
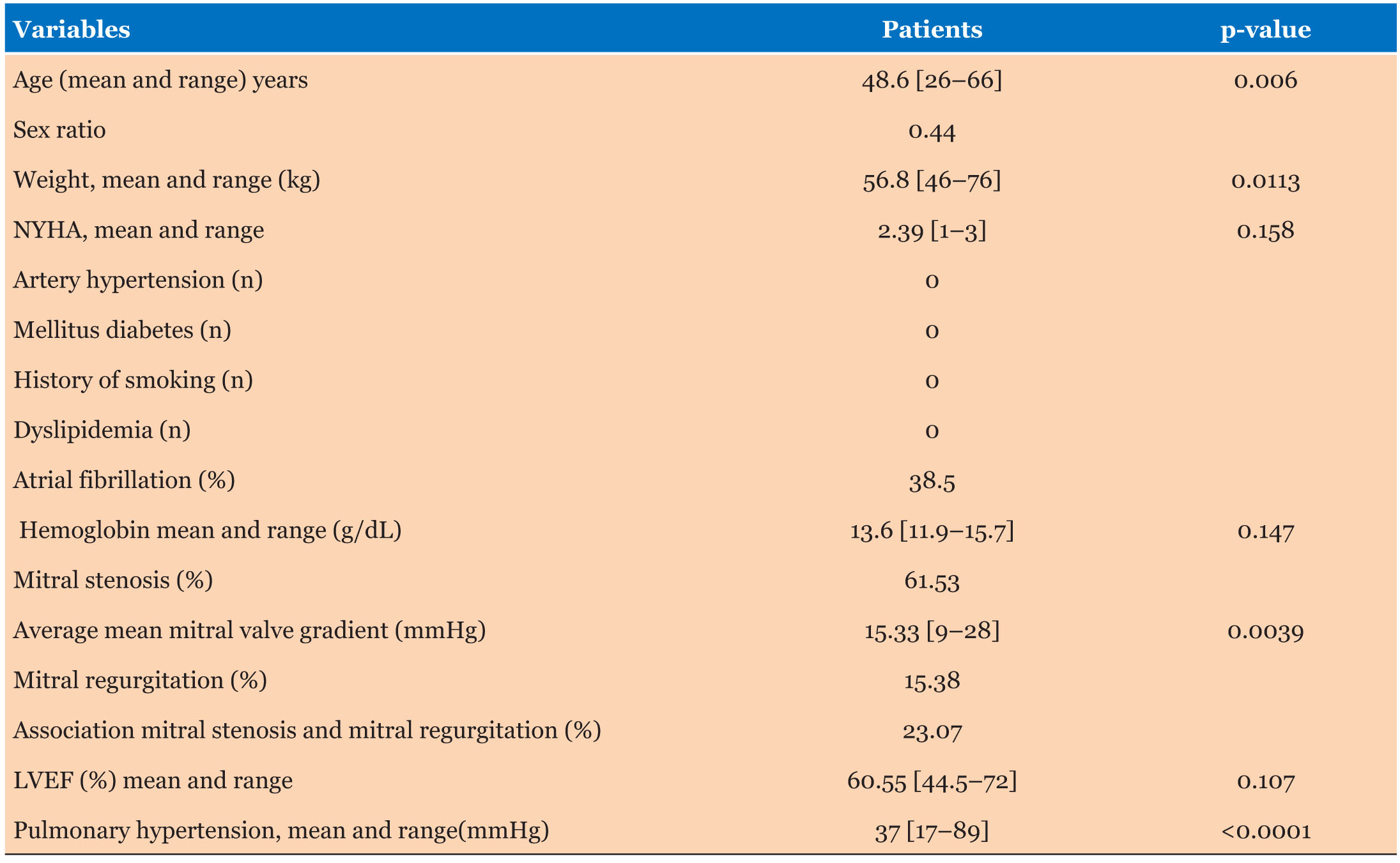
Pre-operative Data (Table 1)
The mean age of our patients was 48.6 [26–66] years, mean weight 56.8 [46–76] g, the sex-ratio at 0.44. The average New York Heart Association was 2.39 [1–3]. All the patients did not have heart risks factors such as diabetes, health technology assessment (HTA), dyslipidaemia, history of smoking. The electrocardiogram showed that 38.5% of the patients had atrial arrhythmia. The valvular lesions were dominated by mitral stenosis in 61.53% of cases, the mean left ventricular ejection fraction (LVEF) was 60.5% [44.5–72], and the average mean mitral valve pressure gradient was 15.3 [9–28] mmHg. The mean pulmonary hypertension was 37 [17–89] mmHg.
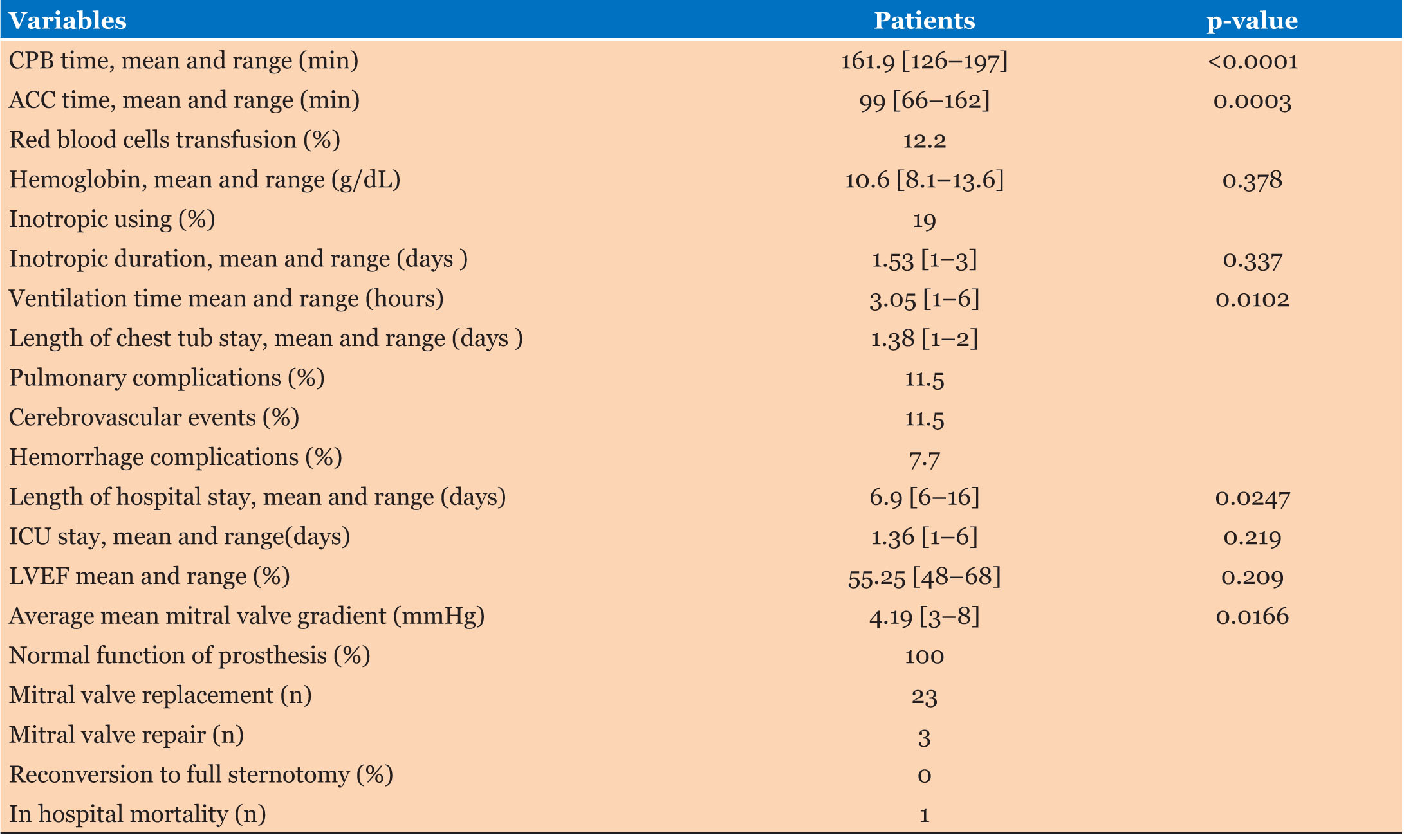
The biologic report showed 13.6 [11.9–15.7] g/dL as mean hemoglobin. Right anterior mini-thoracotomy (RAMT) with femoro-femoral cannulation for CPB was the surgical approach in all the patients. The majority (84.6%) received mitral valve replacement using mechanical prosthesis. Three (3) patients underwent mitral valve repair. Conversion to full sternotomy was not performed in any case, there were no major complications. In intra-operative and post-operative, 12.2% of the patients received red blood cells transfusion for bleeding and the mean post-operative hemoglobin before transfusion was 10.6 [8.1–13.6] g/dL (Table 2). Among our patients, 19% needed inotropic support administration with duration from 1 to 3 hours. The mean CPB time and the one of the aortic cross clamp (ACC) were respectively 161 and 99 minutes. The post-operative course was uneventful. In fact, the mean time of the ventilation was 3.05 [1–6] hours; chest drains were removed in average 1.3 days post-operative. The mean time of ICU stay was 1.1 [1–6] days, the length hospital stay was 6.9 [6–16] days. There was no atrial or ventricular arrhythmia, no chest wound infection. TEE data showed 55.5% [48–68] as a mean LVEF and the average mean mitral valve pressure gradient was 4.9 [3–8] mmHg. However, 11.5% of the patients had minor cerebrovascular events and 11.5% had pleural effusion which needed surgical chest drainage. Moreover, we notified one in-hospital death due to pulmonary failure.
DISCUSSION
Minimally invasive mitral valve surgery is among new surgical approach which might reduce surgical trauma, length of hospital stay in mitral valve surgery. In this discussion we try to compare our series to the literature with reference to patient selection, surgical techniques, and post-operative outcomes.
In our series, pre-operative data showed that our patients were younger (median 48.6 years, range [26–66]) without surgical risks. The TTE revealed good heart function based on left ventricular ejection fraction (LVEF 60.5% [44.5–72]); the atrial fibrillation was found in 38% of the patients. In addition, the average of pulmonary pressure was 37 [17–89] mmHg.
Our baseline of patient characteristics is not so far from those reported by Gammie et al. [8], Liu et al. [9] who reported respectively 59 years as mean age, and 50.57±11.78 years as an interquartile range. However Chen et al. [10] reported elderly patients in their series (interquartile range 68±2.6) years. All these studies reported patients with good left ventricular function.
They reported also pre-operative atrial fibrillation in respectively 12%, 28, 1%, and 51%, 49%. Cardiac arrhythmia should not be contraindications of MIMVS.
As our study, mild to moderate pulmonary artery pressure was reported by Chen et al. [10] (range 66.5±9.6) mmHg and Liu et al. [9] (range 49.70±18.03) mmHg. Mild to moderate pulmonary artery pressure should not be contraindication in MIMVS. Our observation confronted to those of authors cited above is consistent with valvular heart disease management according to the ACC/American Heart Association (AHA) guidelines [4]. Additionally, these observations show that MIMVS can be performed whatever the age in patient without potential surgical complications. Patient’s selection for MIMVS is now beyond patients with high surgical risk. The ideal patient may be a patient without high surgical risk because this technique may increase the time of surgical procedure.
In our series the mean post-operative haemoglobin was 10.6 and 12.2% of patients received red blood cells transfusion. Gammie et al. [8] and Liu et al. [9] in their comparative studies reported respectively 41%, and 23.27% (intra-operative transfusion) as incidence of red blood cells transfusion.
The mean time of mechanical ventilation in our study was 3 hours, range [1–6] which is less than those reported by Liu et al. [9], (15.29±11.45) hours, Chen et al. [10] (21.4±6.1) hours. This difference may due to the fact that our population was little younger.
The time of ICU stay reported in our series was 1.1 [1–6] days and the hospital length of stay at 6.9 [6–16] days. Our results corroborate with those reported by Chen et al. [10], 2.2±1.4 days (ICU), 10.5±2.9 days (hospital stay) and Liu et al. [9], 44.12±39.59 hours (ICU), 5.64±1.75 days (hospital stay).
The length of chest tub stay in our study was 1.38 [1–2] days which is similar to the time reported by Liu et al. [9], 2.59±1.75. The less duration of mechanical ventilation, chest drainage, and ICU stay allow early ambulation and thus faster recovery.
Less of our patients had need inotropic support administration (19%) that means there was no heart failure in the post-operative course. This observation is consistent with the series of Chen et al. [10] in which any case of heart failure was reordered.
The mean CPB time and aortic cross clamp time were respectively 161 and 99 minutes. Our results corroborate with the study of Liu et al. who reported 145, 97±34.65 minutes as CPB time, and 93.89±25.25 minutes as aortic cross clamp time. As the studies of Liu et al. [9], Chen et al. [10], we did not recorder any chest wound infections but one in-hospital mortality due to pulmonary insufficiency post-inflammatory was notified. In addition a case (11.5%) of pleural effusion was also recorded which have need chest drainage.
In term of arrhythmia, the incidence of cerebrovascular events was 11.5% in our series (case of awakening delay). Liu et al. [10] reported 0.99% of stroke. The reduced surgical field with its theoretically inadequate exposure was advocated as the main cause for possible negative neurologic outcomes. Although early series seem to suggest an increased cerebrovascular events rate, the use of transesophageal echocardiography and continuous CO2 insufflation has recently allowed the achievement of comparable outcomes [11].
Minimally invasive mitral valve surgery may be surgical innovations which improve early post-operative outcomes according to our series and numerous studies.
CONCLUSION
Minimally mitral valve surgery by right anterior mini-thoracotomy can be performed safely without additional operative complications. It may improve early post-operative outcomes. A comparative study with conventional full sternotomy is necessary in order to establish the interest of this new approach.
REFERENCE
1.
Mohr FW, Falk V, Diegeler A, Walther T, van Son JA, Autschbach R. Minimally invasive port-access mitral valve surgery. J Thorac Cardiovasc Surg 1998;115(3):567–76. [CrossRef]
[Pubmed]

2.
Grossi EA, LaPietra A, Ribakove GH, et al. Minimally invasive versus sternotomy approaches for mitral reconstruction: Comparison of intermediate-term results. J Thorac Cardiovasc Surg 2001;121(4):708–13. [CrossRef]
[Pubmed]

3.
Seeburger J, Borger MA, Falk V, et al. Minimal invasive mitral valve repair for mitral regurgitation: Results of 1339 consecutive patients. Eur J Cardiothorac Surg 2008;34(4):760–5. [CrossRef]
[Pubmed]

4.
Bonow RO, Carabello BA, Chattenrjee K, et al. ACC/AHA 2006 Guidelines for the Management of Patients with Valvular Heart Disease: Executive Summary a Report of the American College of Cardiology/American HeartAssociation Task Force on Practice Guidelines (Writing Committee to Revise the 1998 Guidelines for the Management of Patients With Valvular Heart Disease). Circulation 2006;114(5):450–527. [CrossRef]

5.
Carpentier A. Cardiac valve surgery – the “French correction”. J Thorac Cardiovasc Surg 1983;86(3):323–37.
[Pubmed]

6.
Chitwood WR Jr, Elbeery JR, Moran JM. Minimally invasive mitral valve repair using transthoracic aortic occlusion. Ann Thorac Surg 1997;63(5):1477–9. [CrossRef]
[Pubmed]

7.
Deloche A, Jebara VA, Relland JY, et al. Valve repair with Carpentier techniques. The second decade. J Thorac Cardiovasc Surg 1990;99(6):990–1002.
[Pubmed]

8.
Gammie JS, Zhao Y, Peterson ED, O’Brien SM, Rankin JS, Griffith BP. J. Maxwell Chamberlain Memorial Paper for adult cardiac surgery. Less-invasive mitral valve operations: trends and outcomes from the Society of Thoracic Surgeons Adult Cardiac Surgery Database. Ann Thorac Surg 2010;90(5):1401–10. [CrossRef]
[Pubmed]

9.
Liu J, Chen B, Zhang YY, et al. Mitral valve replacement via minimally invasive totally thoracoscopic surgery versus traditional median sternotomy: A propensity score matched comparative study. Ann Transl Med 2019;7(14):341. [CrossRef]
[Pubmed]

10.
Chen Q, Yu LL, Zhang QL, Cao H, Chen LW, Huang ZY. Minimally invasive video-assisted mitral valve replacement with a right chest small incision in patients aged over 65 years. Braz J Cardiovasc Surg 2019;34(4):428–35. [CrossRef]
[Pubmed]

11.
Peters WS, Smith JA, Preovolos A, Rabinov M, Buckland MR, Rosenfeldt FL. Mitral valve replacement via a right mini-thoracotomy in the dog: use of carbon dioxide to reduce intracardiac air. Eur J Cardiothorac Surg 1997;11:1067–73. [CrossRef]
[Pubmed]

SUPPORTING INFORMATION
Author Contributions
Issaka Zallé - Conception of the work, Design of the work, Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Moussa Son - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Mouhcine El Mardouli - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Drissi Boumzebra - Acquisition of data, Analysis of data, Drafting the work, Revising the work critically for important intellectual content, Final approval of the version to be published, Agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Guarantor of SubmissionThe corresponding author is the guarantor of submission.
Source of SupportNone
Consent StatementWritten informed consent was obtained from the patient for publication of this article.
Data AvailabilityAll relevant data are within the paper and its Supporting Information files.
Conflict of InterestAuthors declare no conflict of interest.
Copyright© 2021 Issaka Zallé et al.. This article is distributed under the terms of Creative Commons Attribution License which permits unrestricted use, distribution and reproduction in any medium provided the original author(s) and original publisher are properly credited. Please see the copyright policy on the journal website for more information.